Stefan Flasche, Mark Jit, Isabel Rodrıguez-Barraquer, Laurent Coudeville, Mario Recker, Katia Koelle, George Milne, Thomas J. Hladish, T. Alex Perkins, Derek A. T. Cummings, Ilaria Dorigatti, Daniel J. Laydon, Guido España, Joel Kelso, Ira Longini, Jose Lourenco, Carl A. B. Pearson, Robert C. Reiner, Luis Mier-y-Teran-Romero, Kirsten Vannice, Neil Ferguson
PLOS Medicine
November 29, 2016
ABSTRACT
Background
Large Phase III trials across Asia and Latin America have recently demonstrated the efficacy of a recombinant, live-attenuated dengue vaccine (Dengvaxia) over the first 25 mo following vaccination. Subsequent data collected in the longer-term follow-up phase, however, have raised concerns about a potential increase in hospitalization risk of subsequent dengue infections, in particular among young, dengue-naïve vaccinees. We here report predictions from eight independent modelling groups on the long-term safety, public health impact, and cost-effectiveness of routine vaccination with Dengvaxia in a range of transmission settings, as characterised by seroprevalence levels among 9-y-olds (SP9). These predictions were conducted for the World Health Organization to inform their recommendations on optimal use of this vaccine.
Methods and Findings
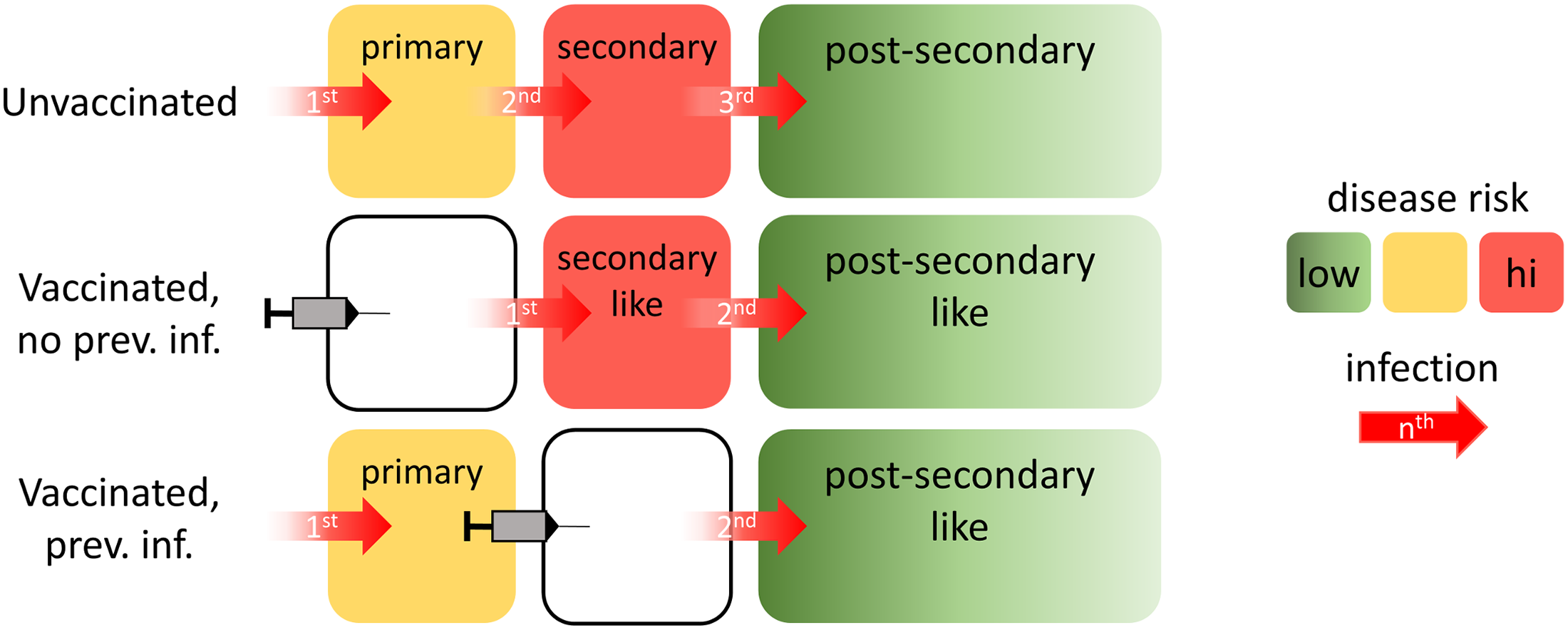
The models adopted, with small variations, a parsimonious vaccine mode of action that was able to reproduce quantitative features of the observed trial data. The adopted mode of action assumed that vaccination, similarly to natural infection, induces transient, heterologous protection and, further, establishes a long-lasting immunogenic memory, which determines disease severity of subsequent infections. The default vaccination policy considered was routine vaccination of 9-y-old children in a three-dose schedule at 80% coverage. The outcomes examined were the impact of vaccination on infections, symptomatic dengue, hospitalised dengue, deaths, and cost-effectiveness over a 30-y postvaccination period. Case definitions were chosen in accordance with the Phase III trials.
All models predicted that in settings with moderate to high dengue endemicity (SP9 ≥ 50%), the default vaccination policy would reduce the burden of dengue disease for the population by 6%–25% (all simulations: –3%–34%) and in high-transmission settings (SP9 ≥ 70%) by 13%–25% (all simulations: 10%– 34%). These endemicity levels are representative of the participating sites in both Phase III trials. In contrast, in settings with low transmission intensity (SP9 ≤ 30%), the models predicted that vaccination could lead to a substantial increase in hospitalisation because of dengue. Modelling reduced vaccine coverage or the addition of catch-up campaigns showed that the impact of vaccination scaled approximately linearly with the number of people vaccinated. In assessing the optimal age of vaccination, we found that targeting older children could increase the net benefit of vaccination in settings with moderate transmission intensity (SP9 = 50%). Overall, vaccination was predicted to be potentially cost-effective in most endemic settings if priced competitively.
The results are based on the assumption that the vaccine acts similarly to natural infection. This assumption is consistent with the available trial results but cannot be directly validated in the absence of additional data. Furthermore, uncertainties remain regarding the level of protection provided against disease versus infection and the rate at which vaccine-induced protection declines.
Conclusions
Dengvaxia has the potential to reduce the burden of dengue disease in areas of moderate to high dengue endemicity. However, the potential risks of vaccination in areas with limited exposure to dengue as well as the local costs and benefits of routine vaccination are important considerations for the inclusion of Dengvaxia into existing immunisation programmes. These results were important inputs into WHO global policy for use of this licensed dengue vaccine.